Understanding Achilles Tendinitis: Symptoms and Diagnosis
Picture this: You’re gearing up for your morning run, the crisp air filling your lungs as you anticipate the familiar euphoria of hitting the trail. But as you push off from your doorstep, a nagging pain stabs at your heel, dampening your enthusiasm and slowing your stride. Or imagine the dedicated dancer, whose every leap and pirouette is shadowed by an unrelenting ache that threatens to end their passion prematurely. Achilles tendinitis can be a stealthy disruptor of active lifestyles, sneaking up and taking hold before you even realize it. In this article, we’ll explore the symptoms and diagnosis of Achilles tendinitis, equipping you with the knowledge to recognize and address this condition before it sidelines you for good.
Early Morning Stiffness: The Day’s First Warning Sign
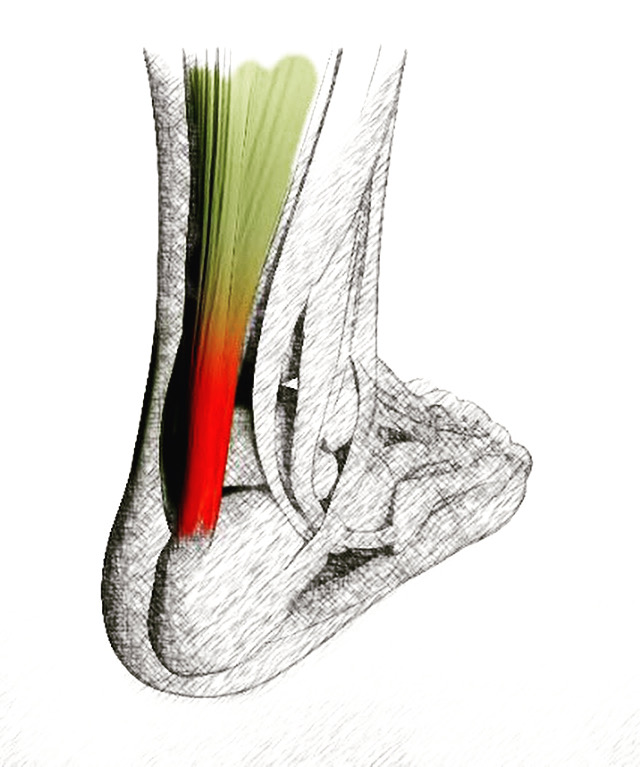
Achilles tendinitis is a common condition that affects the Achilles tendon, which connects your calf muscles to your heel bone. One of the earliest and most telling symptoms of this ailment is early morning stiffness. Upon waking up, individuals with Achilles tendinitis often experience a notable tightness or stiffness in the back of their lower leg. This stiffness is typically most pronounced during the first steps taken after getting out of bed. The discomfort may gradually ease as the tendon warms up and becomes more flexible with movement, but it serves as an important early warning sign that should not be ignored. Recognizing and addressing this symptom promptly can help prevent further damage and complications.
The root cause of early morning stiffness lies in the Achilles tendon’s response to prolonged periods of inactivity, such as sleep. During rest, the tendon tightens and shortens slightly. When you begin to move upon waking, the sudden demand for flexibility and strength from the tendon can reveal underlying inflammation and microtears, resulting in the stark stiffness experienced. This symptom is often accompanied by mild to moderate pain, swelling, or tenderness along the tendon. If these signs persist or worsen, it is crucial to consult a healthcare professional for an accurate diagnosis and appropriate treatment plan. Ignoring these early warning signs can lead to the progression of the condition, making it more challenging to treat and manage.
Diagnosing Achilles tendinitis involves a comprehensive approach that includes a physical examination and potentially imaging tests. A healthcare provider will assess the affected area for tenderness, swelling, and range of motion limitations. They may also perform specific tests to evaluate the strength and function of the tendon. Imaging techniques such as ultrasound or MRI can provide detailed images of the tendon, revealing any inflammation, tears, or structural abnormalities. Early diagnosis is key to managing Achilles tendinitis effectively, as it allows for the implementation of conservative treatments such as rest, ice, compression, and elevation (RICE), along with targeted physical therapy exercises designed to strengthen the tendon and improve flexibility. Addressing early morning stiffness and other symptoms promptly can significantly enhance recovery outcomes and reduce the risk of chronic Achilles tendinitis.

Achilles Tendinitis
Persistent Heel Pain: Beyond Ordinary Soreness
Achilles tendinitis is a condition characterized by inflammation of the Achilles tendon, and one of its hallmark symptoms is persistent heel pain. This pain often extends beyond ordinary soreness and serves as a critical indicator of an underlying issue. Unlike the typical aches experienced after a strenuous workout, the pain associated with Achilles tendinitis does not subside with rest and may even intensify over time. Individuals may notice sharp or burning sensations around the heel, particularly during activities that involve running, jumping, or climbing stairs. This persistent discomfort can significantly impact daily activities and athletic performance, making early recognition and intervention essential.
The underlying cause of persistent heel pain in Achilles tendinitis is typically due to repetitive stress and overuse of the tendon. Microtears and inflammation result from continuous strain, leading to pain and swelling that extend into the heel area. This pain is often most intense in the morning or after periods of inactivity, when the tendon stiffens and then has to quickly adapt to movement. Additionally, factors such as improper footwear, inadequate training techniques, or sudden increases in physical activity can exacerbate the condition. Persistent heel pain should not be dismissed as mere soreness, as it signals a need for medical evaluation and appropriate treatment to prevent further damage.
Diagnosing Achilles tendinitis when faced with persistent heel pain involves a thorough examination by a healthcare provider. During the assessment, the provider will evaluate the tender areas, check for swelling, and test the range of motion in the foot and ankle. They may also inquire about the patient’s activity levels, footwear choices, and any recent changes in exercise routines. Imaging tests such as X-rays, ultrasounds, or MRI scans can provide detailed insights into the extent of tendon damage and inflammation. Early diagnosis is crucial for managing Achilles tendinitis effectively, allowing for targeted treatments like rest, physical therapy, and anti-inflammatory measures. Addressing persistent heel pain promptly can alleviate symptoms and prevent the progression of the condition, ensuring better long-term outcomes and a quicker return to regular activities.
Swelling and Tenderness: Visible Clues
Achilles tendinitis is an inflammatory condition that affects the Achilles tendon, connecting the calf muscles to the heel bone. One of the most visible and palpable symptoms of this condition is swelling and tenderness around the affected area. Individuals experiencing Achilles tendinitis often notice a noticeable thickening or bulging along the tendon, accompanied by redness and warmth. This swelling is typically more pronounced after physical activity or prolonged periods of standing. The tenderness can be felt when pressing on the tendon, especially near the heel, and may vary in intensity from mild discomfort to severe pain. These visible clues serve as critical indicators of underlying inflammation and should prompt individuals to seek medical evaluation promptly.
The onset of swelling and tenderness in Achilles tendinitis is primarily due to repetitive stress and microtears within the tendon fibers. As the tendon endures continuous strain from activities such as running, jumping, or abrupt changes in direction, the microscopic damage accumulates, leading to inflammation and fluid buildup. This response is the body’s natural mechanism to repair the injured tissue but can result in significant discomfort and impaired function. Factors such as overtraining, wearing improper footwear, and insufficient warm-up routines can exacerbate these symptoms. Recognizing and addressing these visible signs early on is crucial to prevent the progression of the condition and minimize the risk of chronic tendinitis or tendon rupture.
Diagnosing Achilles tendinitis based on swelling and tenderness involves a comprehensive evaluation by a healthcare professional. During the examination, the provider will palpate the Achilles tendon to assess the extent of swelling and pinpoint areas of tenderness. They may also evaluate the range of motion and strength in the ankle and foot to determine the impact of the condition. In some cases, imaging studies such as ultrasound or MRI may be employed to visualize the extent of the inflammation and any structural abnormalities within the tendon. Early diagnosis enables the implementation of effective treatment strategies, including rest, physical therapy, and anti-inflammatory measures, aimed at reducing swelling and promoting tendon healing. Addressing swelling and tenderness promptly can lead to better treatment of Achilles tendinitis, facilitating a quicker recovery and return to normal activities.
Achilles Tendinitis Symptoms
Activity-Related Flare-Ups: The Activity-Pain Cycle
Achilles tendinitis is a painful condition affecting the Achilles tendon that often presents itself through activity-related flare-ups. These flare-ups are characterized by a cycle of pain that intensifies with physical activity and subsides with rest, creating a challenging scenario for individuals who are physically active. The activity-pain cycle begins when the tendon, already stressed from repetitive motions or sudden increases in intensity, becomes inflamed. Activities such as running, jumping, or even walking for extended periods can exacerbate the inflammation, leading to sharp or aching pain along the back of the heel and lower leg. This recurrent discomfort often forces individuals to modify or limit their physical activities to manage the symptoms.
The root cause of these activity-related flare-ups lies in the overuse and microtrauma sustained by the Achilles tendon during vigorous activities. When the tendon is exposed to repetitive stress without adequate time for recovery, it undergoes microtears that trigger an inflammatory response. This inflammation leads to pain and swelling, which are typically most noticeable during or after physical exertion. Factors such as improper footwear, inadequate warm-up routines, and biomechanical issues like flat feet or tight calf muscles can further contribute to the susceptibility of the tendon to these flare-ups. Understanding this activity-pain cycle is essential for devising effective strategies to manage and mitigate the symptoms of Achilles tendinitis.
Diagnosing Achilles tendinitis, especially in the context of activity-related flare-ups, requires a thorough evaluation by a healthcare professional. The assessment will likely include a detailed history of the patient’s physical activities, the onset and pattern of pain, and any contributing factors such as changes in workout routines. A physical examination will focus on identifying tenderness, swelling, and range of motion limitations in the affected area. Imaging studies like ultrasound or MRI may be used to confirm the diagnosis and assess the extent of the damage. Early diagnosis and intervention are key to breaking the activity-pain cycle. Treatment plans often include rest, physical therapy, and modifications to activity levels to allow the tendon to heal. By addressing activity-related flare-ups proactively, individuals can reduce pain and improve their chances of a full recovery, enabling them to return to their regular activities without ongoing discomfort.
Limited Range of Motion: A Functional Impairment
Achilles tendinitis is a condition marked by inflammation of the Achilles tendon, commonly leading to a limited range of motion in the affected leg. This functional impairment signifies more than just stiffness; it represents a significant reduction in the ability to perform everyday activities and exercises. Individuals with Achilles tendinitis often experience difficulty in flexing their foot upward or downward, which can hinder walking, running, and climbing stairs. This limitation in movement is typically accompanied by pain and swelling, further exacerbating the difficulty in performing routine tasks. A restricted range of motion not only affects athletic performance but also impacts daily life, making early intervention crucial to prevent long-term disability.
The cause of the limited range of motion in Achilles tendinitis lies in the inflammation and subsequent thickening of the tendon. As the tendon becomes inflamed due to overuse or injury, it loses its elasticity and flexibility. Microtears in the tendon fibers lead to scar tissue formation, which further restricts movement. This loss of flexibility can cause the tendon to become stiff, particularly after periods of inactivity, such as in the morning or after sitting for extended periods. Tight calf muscles and inadequate stretching routines can also contribute to this reduced mobility. Addressing these issues through proper diagnosis and treatment is essential for restoring full functionality and preventing further complications.
Diagnosing Achilles tendinitis with a focus on limited range of motion involves a comprehensive assessment by a healthcare professional. The evaluation includes observing the patient’s gait, testing the ankle’s range of motion, and palpating the tendon to identify areas of tenderness and swelling. Imaging techniques like ultrasound or MRI may be employed to visualize the extent of the injury and inflammation. Early identification allows for targeted treatments such as physical therapy, which focuses on strengthening and stretching exercises to improve flexibility and restore the range of motion. By addressing limited mobility promptly, individuals can achieve better outcomes, reducing pain and enhancing their ability to return to normal activities without restriction.

Achilles Tendinitis Foot Treatment
Risk Factors: Who’s Most Vulnerable?
Achilles tendinitis is a prevalent condition that affects the tendon connecting the calf muscles to the heel bone, and understanding the risk factors can help identify who is most vulnerable to this painful ailment. Athletes, particularly runners and those engaged in high-impact sports like basketball or soccer, are at a higher risk due to the repetitive strain placed on the Achilles tendon. The constant pushing off, jumping, and sudden changes in direction inherent in these sports can lead to microtears and inflammation within the tendon. Additionally, individuals who suddenly increase their activity levels or intensity without proper conditioning are more prone to developing Achilles tendinitis, as their tendons may not be adequately prepared for the heightened demand.
Age is another significant risk factor for Achilles tendinitis. As people age, the tendons naturally lose flexibility and strength, making them more susceptible to injury. Middle-aged adults, particularly those engaging in sporadic physical activity or weekend warriors, often experience a higher incidence of Achilles tendinitis. This demographic might not maintain consistent exercise routines, leading to decreased tendon resilience and an increased likelihood of inflammation when they engage in strenuous activities. Moreover, anatomical factors such as flat feet, high arches, or misaligned gait can contribute to tendon stress, further raising the risk for developing this condition. These structural issues can alter the distribution of forces on the Achilles tendon, leading to overuse and injury.
Certain lifestyle factors and medical conditions also elevate the risk of Achilles tendinitis. Wearing improper footwear, especially shoes without adequate arch support or cushioning, can exacerbate tendon stress. Obesity adds additional strain on the tendons, increasing the likelihood of inflammation and injury. Medical conditions such as diabetes and hypertension can impair blood flow to the tendons, impeding their ability to heal and recover from minor injuries. Understanding these risk factors is crucial for prevention and early intervention. By recognizing who is most vulnerable, individuals can take proactive measures such as adopting appropriate training regimens, wearing supportive footwear, and maintaining a healthy weight to minimize the risk of developing Achilles tendinitis.
Professional Diagnosis: From Self-Assessment to Expert Evaluation
Achilles tendinitis is a condition that affects the Achilles tendon, leading to pain, swelling, and reduced mobility. The path to a professional diagnosis often begins with self-assessment, where individuals notice symptoms such as persistent heel pain, tenderness along the tendon, or stiffness, especially in the morning or after periods of inactivity. These initial signs are crucial for prompting further investigation. Recognizing these symptoms early can lead to timely intervention, preventing the condition from worsening. Self-assessment also involves noting any recent changes in physical activity, footwear, or training intensity that may have contributed to the onset of symptoms.
Once self-assessment indicates a potential issue with the Achilles tendon, seeking expert evaluation becomes imperative. A healthcare professional, typically a sports medicine specialist or an orthopedic doctor, will conduct a comprehensive examination to confirm the diagnosis. This evaluation includes a detailed medical history review to understand the onset and pattern of symptoms, as well as any contributing factors such as past injuries or underlying health conditions. During the physical examination, the doctor will assess the affected area for signs of inflammation, tenderness, and limited range of motion. They may perform specific tests, such as the Thompson test, to evaluate tendon integrity and function.
To gain a precise understanding of the extent of the injury, healthcare providers might utilize imaging techniques such as ultrasound or MRI. These tools help visualize the soft tissues, revealing any tears, thickening, or other abnormalities in the Achilles tendon. Early and accurate diagnosis through expert evaluation enables the formulation of an effective Achilles tendinitis treatment plan tailored to the individual’s needs. This plan may include a combination of rest, physical therapy, and possibly anti-inflammatory medications to reduce pain and promote healing. By transitioning from self-assessment to professional diagnosis, individuals can ensure they receive appropriate care, enhancing their chances of a full recovery and a return to normal activities without ongoing discomfort.

Achilles Tendinitis Treatment
Conclusion
Achilles tendinitis can be a formidable obstacle for anyone who values an active lifestyle, but understanding its symptoms and seeking timely diagnosis can make all the difference. By recognizing early morning stiffness, persistent heel pain, swelling, activity-related flare-ups, limited range of motion, and knowing your risk factors, you can take proactive steps towards addressing the condition. Consulting a healthcare professional ensures an accurate diagnosis and tailored treatment, helping you reclaim your mobility and continue pursuing your passions. Don’t let Achilles tendinitis hold you back—equip yourself with the knowledge and resources needed to overcome this challenge and stride forward with confidence. Here’s to healthier heels and happier trails!
Flagstaff Foot Doctors: Anthony Rosales DPM
https://www.google.com/maps?cid=8835841318590452161
421 N Humphreys St, Flagstaff, AZ 86001, United States
(928) 774-4825
https://flagstafffootandankle.com/
